Two years ago, the Tufts Medical Center Medical Physics department implemented a patient education program called Gray’s Academy. The aim was to help demystify radiation therapy for patients and provide knowledge to help ease their worries.
This week, while we celebrate Patient Safety Awareness Week, we talked to the Tufts Medical Center team about how they built this program and what they’ve learned so far.
How did the Gray’s Academy patient education program get started?
Tufts Medical Center Medical Physicists Chris Melhus, Ph.D., DABR, and Cassandra Stambaugh, Ph.D., DABR, became interested in starting a patient education program after seeing other medical physics teams implementing such programs. Because their team is small, but highly integrated, and because of their own interests in patient care and patient safety, they were compelled to create a program of their own.
As part of their institution’s own overarching quality program, employees could participate in a competitive grant process for programs aimed at improving the patient experience and engagement at their clinic. This grant pushed them to formally put together a plan for their education program with surveys in place to measure the value of the program.
How and when do patients get brought into the program?
Originally, it was planned to be delivered as a group tour for new patients, but due to the pandemic, the team pivoted to a one-on-one program. This turned out to be a benefit. When new patients come to the center, the staff offers the patient a pamphlet with program information and the option for the patient to participate. The patient can then decide if they want to have their education session after CT simulation, on the first day of treatment, or virtually.
What is discussed with the patient during these sessions?
Typically, Dr. Stambaugh or Dr. Melhus start with who they are and what a medical physicist does. Then they give a very high level overview of treatment planning, including targeting the tumor and minimizing dose to OARs, explaining DVH graphs and describing how the MLCs are used. Throughout the discussion, and after the presentation, they open up discussion for the patient’s questions. That becomes a very fluid conversation based on the patient’s concerns – anywhere from general to more technical questions.
Dr. Melhus notes, “This program gives us a chance to be part of the patient care continuum as clinical professionals providing medical services. We can talk to the patient directly about some of the technical aspects that are going to influence their own care. That’s rewarding for us, because we’re also part of that health care journey.”
“This program gives us a chance to be part of the patient care continuum as clinical professionals providing medical services. We can talk to the patient directly about some of the technical aspects that are going to influence their own care. That’s rewarding for us, because we’re also part of that health care journey.”
Chief of Radiation Oncology Physics, Tufts Medical Center
How can patients make sense of medical physics terminology that can seem foreign to them?
The Tufts Medical Physics team aims to speak to the patient in easy-to-understand terms and answer the questions patients have as best they can, based on their specific knowledge. Dr. Stambaugh notes, “With the QA aspect, I keep it very basic. For instance, instead of the term ‘phantom’, I use ‘fake patient’ and I try to use as common language as possible.”
“It’s a process for us too. Talking to patients – there’s no class on that. Part of this to us is becoming better clinicians and relating to patients,” adds Dr. Melhus.
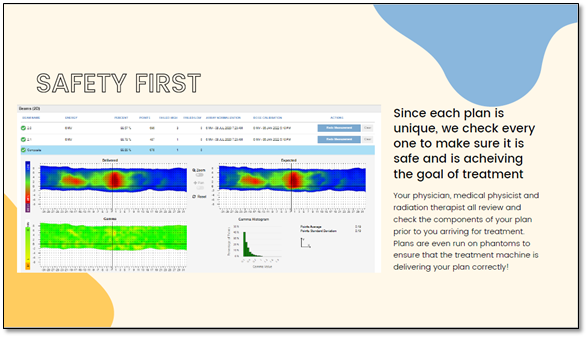
Pictured above: A snapshot of material discussed with patients; shared with permission from Tufts Medical Center
After discussion, the patient is typically shown the treatment delivery system, and the Tufts team finds that showing patients the LINAC helps to solidify the patient’s understanding of the process and the technical aspects.
Dr. Stambaugh observed that, “Patients are comforted by the knowledge that Daily QA is performed every morning before they get on the couch.”
How has the program been received by patients and by others in the department?
For patients, the sessions provide them with knowledge on the unknown aspects of their radiation therapy treatment plan, and that knowledge helps alleviate some of their fears. The Tufts team has also invited patients’ support persons in with them, and that’s been very beneficial. For patients, it can be a very solitary experience, and having their support person come in and understand the process and help them remember all the information, has been really rewarding for everyone.
“For the support person to the patient, they don’t know what happens when their family member enters the room. They just have to sit in the waiting room. So, to have them participate in the session and see the treatment room, creates a higher level of empathy and understanding that doesn’t exist without that experience.”
Medical Physicist & Assistant Professor of Radiation Oncology, Tufts Medical Center
The Tufts team have been blown away by the positive reception of the nursing staff as well. They are very enthusiastic about this program and have become great advocates for it with new patients. Everyone at Tufts has been very supportive and responded positively to the program.
Finally, what has the program brought to the Medical Physicists at Tufts on a personal level?
For the Tufts Medical Physics team, it’s been educational learning how to effectively communicate with patients. It’s also been very professionally rewarding to be really brought into the patient care continuum and to have become a visible part of the patient’s care team.
“It’s been a great and valuable experience on how I can improve as a clinician and contribute to our healthcare mission, and hopefully make a patient’s experience that much better. That’s why we work the long days. It makes the job so much more rewarding,” said Dr. Melhus.
Lastly, on the evolution of the medical physicist, Dr. Melhus notes, “It’s critical for the survival of our profession to not become relegated to be viewed as only a technician. I’m constantly educating upwards on the importance of our role. It’s really key that we communicate our value to the people that make decisions about what happens to our department, our medical staff and our patients.”
About the Tufts Medical Physics Team