In the autumn issue (03/2021) of the EFOMP Newsletter, Jim Malone, Professor (Emeritus) of Medical Physics at Trinity College opined on the SFERA CON SFERA sculpture on campus, stating: “It provides us with a visual metaphor for science, in that the images within the sphere, of surrounding buildings and people are always somewhat distorted. Just as in medical physics. Imperfect representation of reality is the stuff of both science and art.”
As a manufacturer of diagnostic and radiotherapy phantoms, Sun Nuclear fully appreciates the challenges of minimizing distortions, over the lifetime of the phantoms we design and manufacture. A critical element of phantom performance is how well the material used matches human tissue.
Tissue Mimicking Materials (TMM) play a key role in the dose calculations for Treatment Planning Systems, and for absorbed dose estimates in radiographic images studies. For Ultrasound, CT, and Mammography applications, phantoms with exquisite tissue mimicking materials can help to find inconsistencies in imaging system performance.
Ultrasound Tissue Mimicking
For Ultrasound imaging QA, the tissue mimicking material used in Sun Nuclear ultrasound phantoms simulates human tissue speed of sound (SOS) and matches the calibrated SOS (1540 m/sec) of the imaging system itself. The material also shows less variability in acoustic velocity and frequency response due to temperature variations than other phantoms1, impacting geometric accuracy and sensitivity. Recently, the Sono408™ Spherical Lesion phantom found an inconsistency in focal zone settings between two “identical” ultrasound systems (Fig 1).
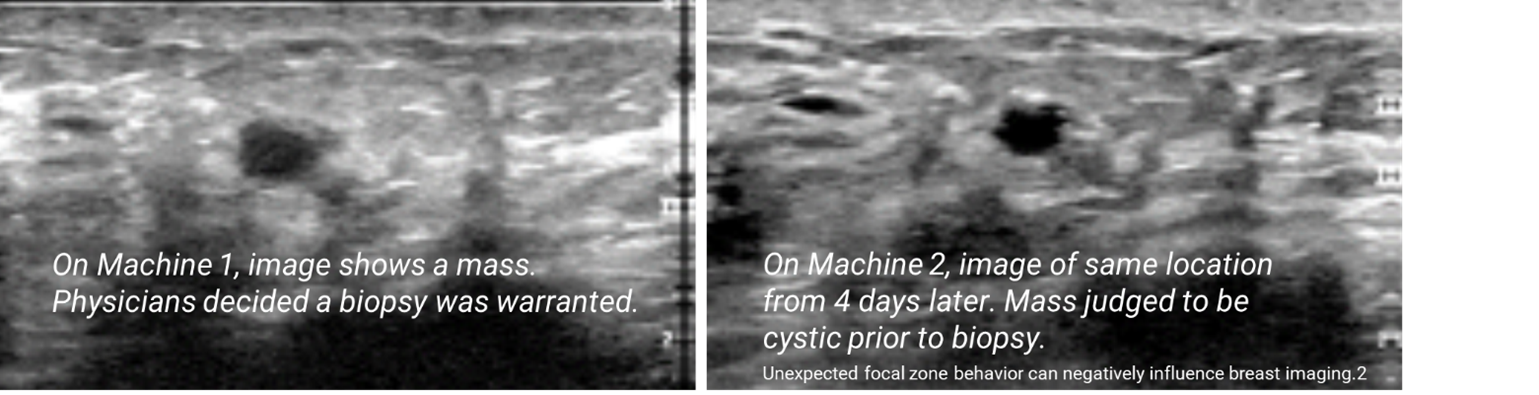
CT for Radiation Therapy Treatment Planning
In radiation therapy treatment planning, CT data is commonly used both to define the patient’s anatomy and to provide tissue density information. Accurate planning, and ultimately delivery, of the treatment is contingent on correctly calibrating the TPS to a CT scanner. Calibrating a Treatment Planning System (TPS) to plastics, rather than patient-like materials, can result in dosimetric errors. Understanding the reasons behind this is key to improving TPS dose agreement.
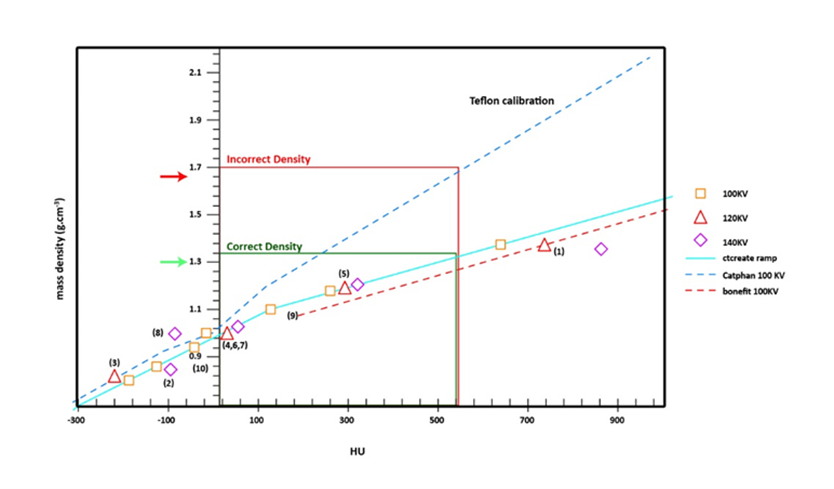
Figure 2, shown above, published by Verhaegen, et al.3 (with example and notes added by Sun Nuclear) shows the difference between planning based upon a calibration using body-like materials versus a calibration curve based on materials such as Teflon and Delrin. Those latter materials have been used as proxies for bone based upon their higher densities, but their effective atomic number, and ultimately HU values, are generally inconsistent with bony tissue. If a TPS is using the lower calibration curve based on ICRU-44 definitions, indicated by the green arrow, a given tissue around 550 HU will map to a patient density of around 1.3 g/cm3. Using the upper calibration curve, indicated by the red arrow, which is based upon Teflon rather than tissue mimicking materials, the TPS would map this same voxel to a density closer to 1.7 g/cm3. The impact of this is overestimating the patient density which would in turn lead to delivering too much energy, resulting in a higher dose than intended. The Verhaegen paper quantified these dose errors in some regions to be up to 10% for 6 and 15 MV photons and 30% for an 18 meV electron beam.3, 4
Mammography Tissue Mimicking
The 2015 EFOMP Mammography Protocol states that “any phantom is a simplified model of clinical reality…”.5 The choice of materials is also evident in Sun Nuclear’s Mammography portfolio. The Modular DBT™ Phantom uses an epoxy resin-based composition that is highly equivalent to the Hammerstein density and elemental compositions of fat, adipose tissue, skin, and Mammary gland.6

It is used for quality control of Digital Breast Tomosynthesis systems. Our high quality breast tissue mimicking material along with the modular design allows for thorough testing and characterization of 2D and 3D systems to EFOMP standards.
In Summary
These phantoms, and the materials they are made of, are examples of Sun Nuclear’s fervent efforts to minimize clinical impact of “imperfect representations of reality”, as Prof. Malone notes on the SFERA CON SFERA. Our comprehensive suite of products and analysis software simplifies workflows for today’s demanding Quality Management needs.
1 J. Browne, et al., Assessment of the Acoustic Properties of Common Tissue-mimicking Test Phantoms. Ultrasound in Medicine and Biology, Vol. 29 (7), pp.1053-1060. 2003.
2 J. Zabzebski, Ultrasound Instrumentation: An Important Focus for the Medical Physicist. 2018 AAPM Spring Clinical Meeting
3 F. Verhaegen and S. Devic, Sensitivity study for CT image use in Monte Carlo treatment planning, Phys. Med. Biol. 50 (2005) 937-9464
4 K. Ruchala, Sun Nuclear Clinical Note, “Calibrate Your Treatment Planning System to Patients, Not Plastic”
5 G. Gennaro, et al., EFOMP Mammo Working Group Protocol, March 2015, Quality Controls in Digital Mammography; http://dx.medra.org/10.19285/M...
6 Hammerstein R., Miller D., White D., et al; Absorbed Dose in Mammography; RADIOLOGY;130:485-491
This article was originally published in the European Federation of Organisations for Medical Physics (EFOMP) Winter 2021 Newsletter. Find the full newsletter here.